If you find this post interesting and think others might do so, spread the word.
I’ve been working at a local vaccine hub over the weekend. It’s been an interesting return to ‘frontline’ practice as a pharmacist, not least because I keep meeting old colleagues and former students. Everyone is tired, so it is a good thing the lockdown appears to be having a great effect on case numbers and hospitalisations, and the vaccine effect is starting to kick in the older age groups.
Talking to patients who have concerns about the vaccines, mainly around ingredients other than the mRNA, has also been fun, but I’m still meeting and hearing of healthcare professionals who haven’t had the vaccine yet, and The Times is reporting over 200,000 frontline NHS staff have not been vaccinated.
But an analysis of official figures reveals that large numbers have still not been vaccinated. Overall, 91 per cent of frontline NHS staff and 72 per cent of care home workers have had a first dose. These figures mask considerable regional variations: about 97 per cent of frontline NHS staff have been vaccinated in the northeast, compared with 76 per cent in London.
The concerns I have heard aren’t much different from the ones that the public have had, including the rumours from social media.
The relative speed of development of the vaccines seems to be the sticking point for some, who are waiting to ‘see what happens’. I’m convinced that part of this comes what we each about the process of drug development at undergraduate level, often highlighting the difficulties and time it takes. There was also some understandable downplaying of expectations about vaccines early in the pandemic that may have stuck in the public consciousness. A private chat with a friend also brought up the fact we are continually told something to cure [insert your disease of choice] will be along in 3-5 years to to cure the disease. It never comes, so the fact this one came within a few months makes people skeptical about it, especially if they are ignorant of the prior work that was leveraged to get the vaccines so quickly.
For healthcare professionals though, I still find it shocking. I think we perhaps need to do more to during undergraduate education to avoid this in future. I haven’t got a fixed view on this, and it goes against my general view on public vaccination, but mandatory COVID-19 vaccination for healthcare professionals looks like a morally defendable position.
Vaccine Hesitancy
There’s a couple of publications about vaccine hesitancy that are worth a read. Chevallier et al offer three recommendations, including testing communications campaigns (pre-registered study designs), using behavioural insights [your mileage may vary on the utility of psychology to deliver] to make vaccination accessible (most of which I think the UK vaccination system has covered), and leveraging the power of social norms.
Have you seen a vaccine card on social media? Got vaccine envy? Good! One of the side benefits of the delayed dose strategy in the UK is that is doubled the expansion of the people spreading vaccination as a social norm. Chevalier et al also note that many initial refuseniks change their mind. This appears to be true…
Since, public support for vaccination in the UK is rising.
Ben Ansell, Professor of Comparative Democratic Institutions at the Department of Politics and International Relations, says, ‘This multi-wave study gives us a rare glimpse of whose opinions have shifted and why. People have become massively more supportive of taking the vaccine overall but important gaps remain especially among groups whose trust in politicians is typically lower: non-voters, younger citizens, and poorer households.’
Even though there are gaps that need addressing, In most cases the norm is to be pro-vaccination. I really think that is the message that needs to be got across. It is too easy to accidentally suggest that the norm is the opposite.
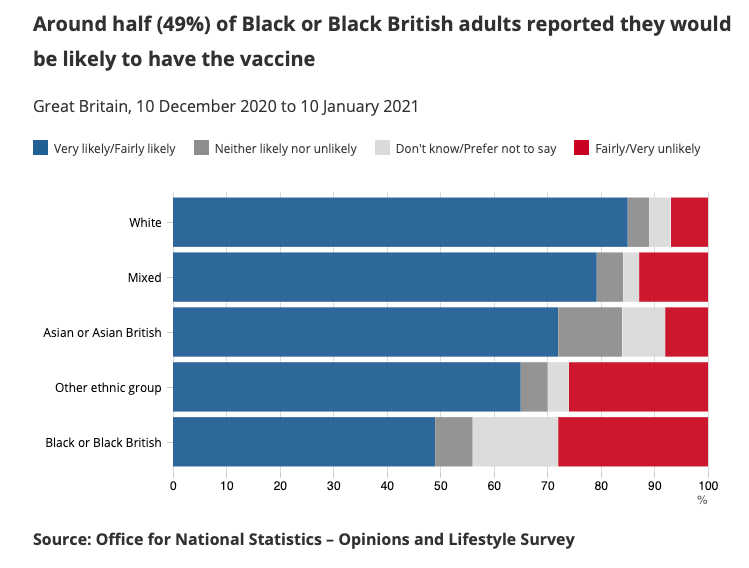
I found this graph from the more detailed report of the study very reassuring.
The ONS note over 90% of people would be likely to have the vaccine if offered, but they do report differences in ethnicity. Black or Black British are a particular concern, although hopefully this position may be better in the end (see above).
20 million people have been vaccinated now. There are no significant safety signals arising. The benefits of the vaccines will start to be seen in combining weeks. Let’s be optimistic and hope that positive views become even more common.
Prioritisation
The JCVI have set out their plan to carry on working down through the age groups, and the clinically vulnerable. If you have worked in a vaccine hub screening area, you’d be aware of just how difficult it is to use any criteria other than age. Even determining frontline status in some people can sometimes be awkward, and people have been turned away who got hold of a link they should not have been forwarded. Your GP doesn’t know your job either. Any supposed benefit would be lost in the bureaucratic nightmare of running anything more complicated. There’s also an interesting paper demonstrating focusing on age saves the most lives, when applied to US, German, and South Korean data.
Faxes cost lives
This piece on the comparative failure of Germany’s vaccination campaign is interesting for multiple reasons, but faxes might surprise you. In the UK, Matt Hancock made faxes ‘illegal’ in 2018 in the NHS, but in Germany they are surprisingly not well digitalised and still use thousands of faxes.
Take the fax machines. A technological dinosaur elsewhere in the West, fax machines remain a mainstay in many medical practices and government health offices. That has made coordination across Germany’s nearly 400 health offices particularly difficult. Health Minister Jens Spahn has spent millions trying to put German health care online, so far with only mixed results.
The fax is merely a symptom of a deeper problem, however. Angela Merkel has talked for years of the necessity to “digitalize” German society, a goal that many other advanced economies have long made a reality. Indeed, the first thing many new arrivals in Germany notice is its lack of connectivity, from the dearth of free Wifi in cafes and restaurants to slow internet speeds. The fact that the German federal government itself still employs nearly 1,000 fax machines in its various ministries tells you everything you need to know about how successful Merkel’s digital revolution is.
That said, the 1970s technology is comparatively modern to the pen and paper still in use across Germany’s medical profession. That a government can’t rely on antiquated communications tools to immunize Germany’s 83 million inhabitants quickly should be obvious.
There are also issues around data privacy concerns…
Denmark is going great guns, and unlike the UK is in the EU scheme so can be compared directly with Germany. They are well above the EU average and should be done by June. Part of this is they are banging out single doses, and not holding vaccine back for second doses as some countries are, but also because Denmark isn’t using faxes…
A highly organised and digitised healthcare system in Denmark is key. Aarhus University professor and virologist Soren Riis Paludan points out that on a typical day, Denmark tests 150,000 people for Covid-19. (For comparison, with a similar population size the Republic tested 105,400 people in the past week.)
A digital ID database that public authorities use to communicate with citizens about everything from pensions to daycare places will help the vaccination plan. It means authorities can sort citizens by age, and send out vaccination invitations directly to their mandatory digital inbox.
BMJ Webinar on vaccines
If you have time, this BMJ webinar is worth watching, if only for Ben Goldacre’s comments about lockdown hair at 55 seconds.
The real highlights for me were Susanne Hodgson’s overview of the vaccines at 6:30, Ben Goldacre’s talk on OpenSAFELY at 25:37 (which I think is an amazing piece of work in terms of size and the methods), and Rick Malley on the vaccine dose schedules at 38:31. Well worth a listen.
That’s all folks. Stay safe.
Anthony
Don’t forget to report your suspected adverse effects from medicines and vaccines. In the UK, this means using the Yellow Card Scheme