If you find these posts interesting and think others might do so, spread the word
To start, a brief mention about the AstraZeneca vaccine…. The MHRA Yellow Card figures have been updated… (13th of May release). It doesn't change any of the MHRA/JCVI assessments/advice…
Up to 5 May 2021, the MHRA had received Yellow Card reports of 262 cases of major thromboembolic events (blood clots) with concurrent thrombocytopenia (low platelet counts) in the UK following vaccination with COVID-19 Vaccine AstraZeneca. These events occurred in 149 women and 112 men aged from 18 to 93 years and the overall case fatality rate was 20% with 51 deaths. Eight cases have been reported after a second dose.
The highlight about second doses is mine. Given that the estimated number of first doses of AstraZeneca Vaccine doses up until the 5th May was 23.3 million, second doses at 7.5 million, the reporting rates are roughly:
First Dose: 1 in 89,000
Second Dose: 1 in 937,500
There has been prior suggestions (when second dose cases were at 4 cases) that the second dose case reports were in individuals with multiple confounders, which I think this tweet hints at:

Even without that knowledge, the cases after second dose are extremely rare (effectively 1 in a million) and should not be a major concern in any normal understanding of dealing with risks. At around 1 in 100,000 most humans start to consider risks as negligible. I’ve had young at risk people in my own family receive AstraZeneca Vaccine, including second doses, and it hasn’t put them off.
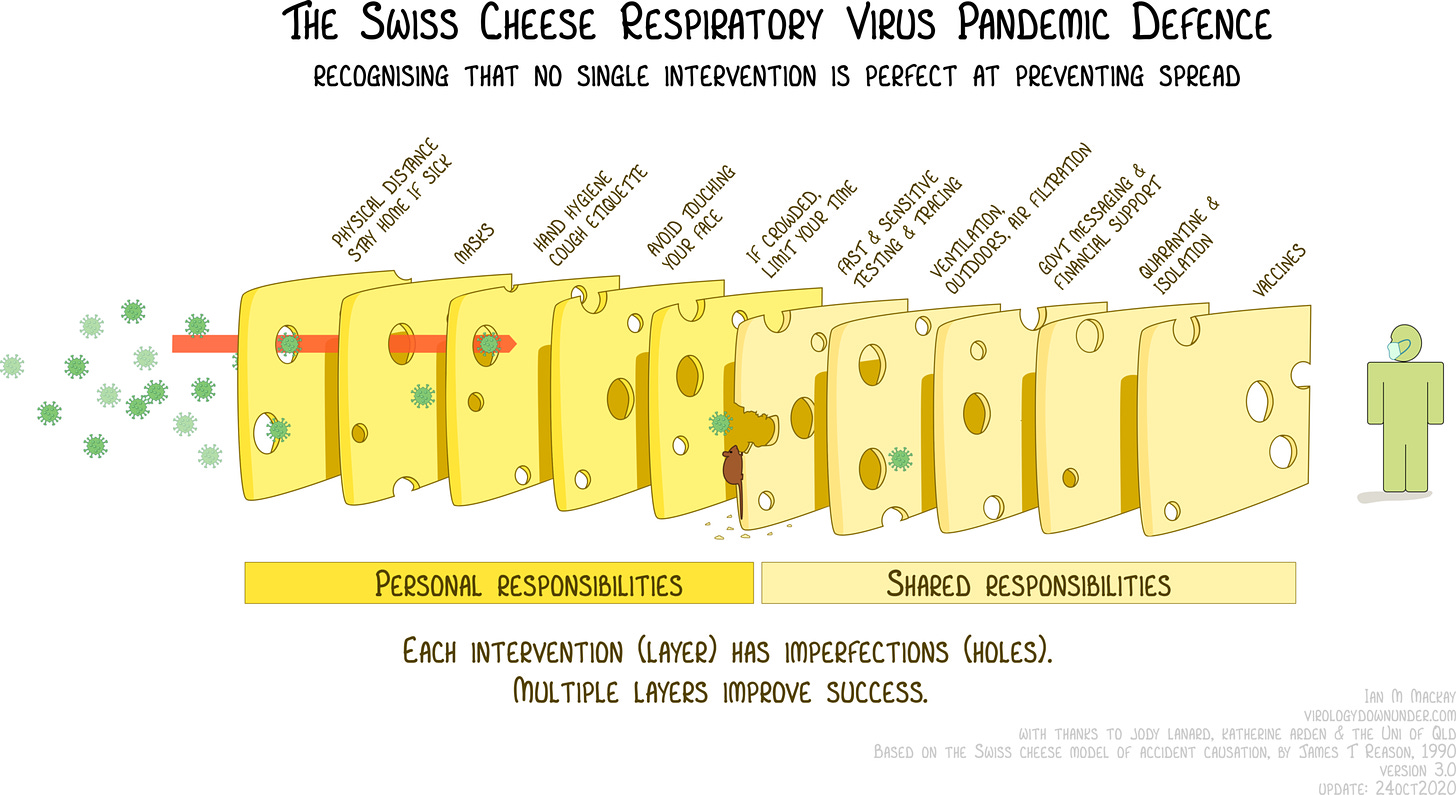
I was sent this graphic, which has also appeared on the appropriate Wikipedia page for James Reason’s cheese model.
Personally, I think the holes are too big in the final slice of cheese representing the vaccine, and that slice ought to be a reasonably thick slice of Parmigiano-reggiano if we are thinking of risk at an individual level.
If we are thinking of population level, with hesitancy, partial vaccine roll out, and the Indian variant, then keep the slice of Gouda.
Reason’s model has been on my mind for another reason this week. I’ve been getting involved with some work around double-checking.
In my own professional area of pharmacy, having two independent individuals checking dispensed medicines in a pharmacy environment is fairly standard practice. It is all too easy to convince yourself you are right when checking yourself due to confirmation bias. Essentially, the second independent check puts in another slice of cheese in the model above, meaning that it is less likely an error will end up in the final dispensed medicine. Your colleague may find the amiloride you dispensed was actually amlodipine. This is pretty much standard practice in pharmacy (unless you are on call).
In the administration of medicines on hospital wards, there has been debate about the utility of double-checking to reduce administration errors of medicines within hospitals. A systematic review 1 in 2020 found that there was insufficient evidence to show any differences in error rates between single and double checking. In the conclusion the authors stated:
Double checking presents at face value as a logical safety precaution which has been embedded in nursing practice for decades. However, as this review reveals, there is no solid evidence-base to support its use. Our review of the evidence shows both an absence of good-quality studies, and generally an absence of effectiveness in reducing medication error rates and patient harm. In most studies, the double-checking process tested was ill-defined and the fidelity of the double-checking process left un-investigated. Given the extent to which it is embedded as part of routine nursing practice, and the considerable costs involved, there would appear to be a compelling reason to establish a sound evidence-base for its ongoing use and to inform decisions about when and how it might be most effective to improve medication safety.
Personally, I think you’d need good evidence to decide to remove the second check. Mistakes in drug administration can be fatal. That said, double checking is not without problems. George Bartram was a 15 day old baby who was given the wrong dose of digoxin, which led to his death. Two nurses were involved in the administration of the drug:
Blaming pressure and time on the ward, Ms Fitzsimmons said: "Because we had calculated it both separately and together and checked it to make sure it was accurate to the book, we believed that we were giving the right dose.
"If we had any doubt whatsoever we would not have given the dose."
An editorial by Pfeiffer et al2 that accompanies the systematic review above discusses the concept of double checking (and proposes a framework for creating stronger research evidence). At one point they state about double checking:
If it is carried out by two people (compared with a technology-based check, like barcode scanning), the detection rate is limited because both people may be affected by the same disturbances in the environment, for example, noise, confusing drug labels or cognitive biases in information processing (eg, confirmation bias). Double checks also may become a mindless routine over time, meaning that the checking persons rely on the other check and are not as attentive as they could be. In addition, checking persons may not dare to raise an identified error to a person of higher authority status.
All of that makes sense, but I do think you have to be careful before discarding the double check.
It would also be interesting to compare nursing and pharmacy double checks. Perhaps double checks in pharmacy are easier to carry out since the environment is more controlled, with less distractions than a hospital ward. The process of dispensing is more physically and temporally separated, and slightly more like a pseudo-manufacturing process. For this reason the second check is likely more independent, with the checker coming to it new without priming by a colleague. On a nurse administration round, two individuals will be working together as they go round the ward, seeing information at the same time. That separation of process is much harder in such circumstances. All very interesting.
Sometime ago, our team did some work on medication errors in Coroner’s reports.3 4 It’s been great to see others build on this. Anis et al have a preprint out concerning deaths related to the use (or lack of use) of anti-coagulants found in coroner’s reports.5 A median of 16 such cases were reported per year, most involving warfarin, with issues around poor systems, poor communication, poor medical records and failures or delays in appropriate assessments being the most reported coroner concerns. Most of the lessons learned about these cases didn't go beyond the local NHS, which is a finding we also saw.
That should change.
That’s all and stay safe.
Anthony
Don’t forget to report your suspected adverse effects from medicines and vaccines. In the UK, this means using the Yellow Card Scheme.
Koyama AK, Maddox CS, Li L, et al Effectiveness of double checking to reduce medication administration errors: a systematic review BMJ Quality & Safety 2020;29:595-603.
Pfeiffer Y, Zimmermann C, Schwappach DLB What are we doing when we double check BMJ Quality & Safety 2020;29:536-540.
Ferner RE, Easton C, Cox AR. Deaths from Medicines: A Systematic Analysis of Coroners’ Reports to Prevent Future Deaths. Drug Saf [Internet]. 2018;41(1):103–10. Available from: https://doi.org/10.1007/s40264-017-0588-0
Ferner RE, Ahmad T, Babatunde Z, Cox AR. Preventing Future Deaths from Medicines: Responses to Coroners’ Concerns in England and Wales. Drug Saf [Internet]. 2019 Mar 7 [cited 2021 Apr 17];42(3):445–51. Available from: https://doi.org/10.1007/s40264-018-0738-z
Anis A, Heneghan C, Aronson JK, DeVito NJ, Richards GC Deaths from cardiovascular disease involving anticoagulants: a systematic synthesis of coroners’ case reports to prevent future deaths medRxiv 2021.04.28.21256272; doi:https://doi.org/10.1101/2021.04.28.21256272